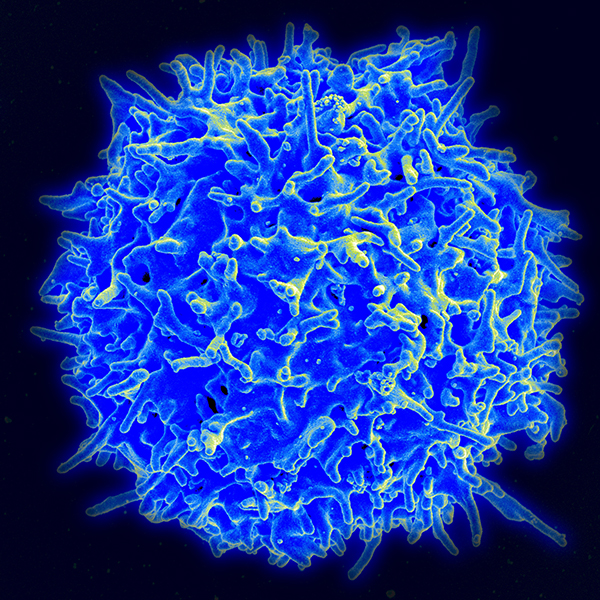
A healthy T cell (Image courtesy of the National Institute of Allergy and Infectious Diseases)
USC PhD student Lisa Nguyen and colleagues in the laboratory of Rong Lu observed this phenomenon by tracking the individual blood stem cells that reside in the bone marrow of mice. To create the tracking labels, the scientists attached a unique piece of genetic code to each blood stem cell. During blood production, each blood stem cell passes its unique genetic label onto its progeny—which include two types of immune cells, known as B cells and T cells.
To test the contributions of these uniquely labelled blood stem cells, the scientists performed a series of bone marrow transplantations in mice. Mice received a combination of normal blood stem cells and deficient blood stem cells with a genetic mutation that prevented them from producing either B cells only, or both B and T cells.
The scientists found that the normal blood stem cells compensated for the B and T cell deficiencies. When co-transplanted with B-deficient stem cells, the normal stem cells overproduced B cells to keep the immune system in balance. And when co-transplanted with B- and T-deficient stem cells, the normal stem cells compensated by overproducing both B and T cells to maintain a balanced immune system.
Furthermore, the scientists found that a few specific blood stem cells were doing most of the work. These key blood stem cells proliferated dramatically to compensate for the immune cell deficiencies in the recipient mice, and these cells continued to proliferate when they were transplanted into different recipient mice. Furthermore, these highly productive blood stem cells showed changes in gene activity that enhanced their ability to oversupply deficient types of immune cells.
“These stem cells’ ability to compensate provides some degree of resilience to disruptions of the blood and immune system—such as the aging process, the early stages of many blood cancers and disorders, and bone transplantation,” said Lu, an assistant professor of stem cell biology and regenerative medicine at USC. “By understanding and ultimately harnessing this innate capacity of stem cells, we can potentially optimize treatments for a wide range of diseases.”
Additional co-authors include Zheng Wang, Adnan Y. Chowdhury, Elizabeth Chu, Jiya Eerdeng and Du Jiang from the Lu Laboratory.
Funding came from the National Institutes of Health (R00HL113104, R01HL135292, R01HL138225, P30CA014089, T32HD060549, and F31HL134359), the Rose Hills Foundation Science and Engineering Fellowship, the USC Provost’s Undergraduate Research Fellowship, the California Institute for Regenerative Medicine Training Grant, the Hearst Fellowship Award, the USC Office of Research, and the Norris Medical Library.
– Cristy Lytal