By Diane Krieger
A spinning chair equipped with head straps, recording goggles and seatbelt. An overhead screen displaying magnified images of your eyes, responding in real-time to stimuli. Other goggles to measure activity in the five balance organs or to record the inner ear’s reaction to subtle changes in water temperature.
Alaina Bassett, AuD, PhD, is the gatekeeper to these and other technology-driven diagnostic tools used in the assessment of vestibular disorders, a dizzying array of conditions affecting balance in some 33 million Americans a year.
Bassett heads up the USC Balance Center.
First launched in 2018, with Bassett as founding director, the center conducts up to a dozen patient evaluations a week.
“I’m an audiologist with a background in vestibular assessment and balance function,” says Bassett, a clinical assistant professor in the USC Caruso Department of Otolaryngology and Head and Neck Surgery at the Keck School of Medicine of USC. “My job is to manage and help patients with symptoms of dizziness and unsteadiness.”
What makes Keck Medicine of USC’s balance center unique is its approach. After each assessment, Bassett assembles the multidisciplinary team to tackle that patient’s case.
“Typically patients with dizziness have already seen three or four doctors before coming to me,” Bassett says. “They’re tired of being pushed around. So we really want to make sure we’re able to triage effectively — where they can walk out of here feeling good about themselves.”
Vestibular dysfunction is complicated. There are more than 25 common causes of balance disorders, ranging from pharmacotoxicity to head trauma, from inherited conditions such as Ménière’s disease to complications related to aging, autoimmune disease or allergies.
Because balance affects people across the lifespan, Bassett sees patients “from 4-year-old children to the very oldest senior citizens.”
While the USC Balance Center is brimming with state-of-the-art equipment, Bassett also relies on “old school” strategies. Her detective work begins in the waiting room.
“I’m evaluating your balance system as soon as I see you,” she says. “Are you using a cane? Have your glasses slid down the bridge of your nose? Are they crooked? Are they bifocals? I’m always watching, observing and, above all, listening — because people are very good historians. They’ll mention things about their personal or professional lives that can be really important.”
Bassett devotes time to educating patients. She introduces them to the labyrinth, a maze-like structure of bone and soft tissue within the inner ear. She’ll explain how the five vestibular organs on each side of the head interact with the brain, the eyes and other body systems, right down to the muscles and touch sensors in the legs and feet.
“I ask many questions and make patients repeat things, just to double-check, because it can really help us make the right decisions for them moving forward.”
She then proceeds to put patients’ balance organs through their paces.
“It’s a full-service experience,” she says of the workup.
Balance Assessment Primer
Patients visiting the Balance Center get a two-hour evaluation involving a series of eye movement tasks, head movement tasks and other specialized tests focused on all five balance organs.
Here’s what to expect:
Videonystagmography is a basic vestibular assessment that allows Bassett to observe, record and play back a patient’s ocular movements under different stimuli. VNG is the frontline tool in detecting nystagmus, a class of vision disorders causing the eyes to make repetitive, uncontrolled motions.
VEMP, short for vestibular evoked myogenic potentials, is an electrophysiology assessment tracking how specific balance organs respond to sound stimulation.
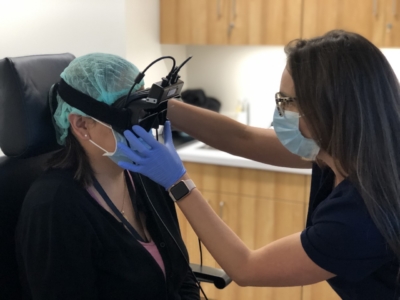
vHIT, short for video head impulse testing, measures peripheral balance deficits. Goggles worn by the patient during this assessment let Bassett accurately measure the function of all six vestibular canals while she manually applies quick turns to the patient’s head.
In rotational chair testing — or what Bassett, to the delight of her younger patients, calls “the spinning tea cup” — the patient revolves at a speed of 180 degrees per second in pitch darkness, strapped in and wearing goggles. This test distinguishes between dizziness caused by disorders of the inner ear and those of the brain.
Because it often induces feelings of motion-sickness in patients, Bassett saves the caloric test for last. By placing warm and cool water in the patient’s ear canal, she can use this test to map the responsiveness and symmetry of a patient’s peripheral vestibular systems.