According the research, children genetically predisposed to overproduce lymphocytes in relation to other white blood cells are at higher risk for pediatric ALL.
By Joanne Shen
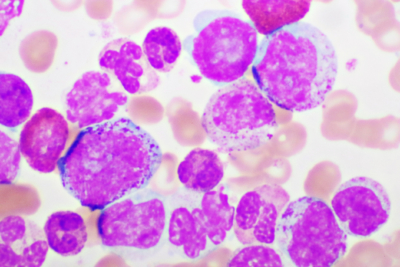
Acute Lymphoblastic Leukemia (ALL), a cancer involving white blood cells known as lymphocytes, is the most common childhood cancer, representing 25% of all cancer diagnoses. It’s also one of the leading causes of childhood cancer deaths. While cure rates have improved thanks to chemotherapy, the cancer treatments are toxic. Survivors face increased risk of heart disease, lung disease, neurocognitive defects as well as increased risk of developing a secondary cancer in their lifetime.
Now, new research published in the American Journal of Human Genetics reveals children born with a genetic predisposition to produce more lymphocytes, particularly in relation to other types of white blood cells, are at a higher risk of developing ALL. This finding could help in the development of risk models for newborns that could lead to early intervention strategies.
“I hope that our research will be able to help to identify children at birth who have the highest risk of leukemia,” says corresponding author Adam de Smith, assistant professor in the Center for Genetic Epidemiology at the Keck School of Medicine of USC and a member of the USC Norris Comprehensive Center. “An ideal goal would be if newborn screenings in the future could incorporate screening for pre-leukemia.”
Past genetic studies identified over a dozen locations on the genome associated with childhood ALL. Noting these spots matched places on the genome associated with variations in blood cell traits, such as white blood cell counts, the USC team was inspired to investigate a connection between overproduction of lymphocytes and the risk of developing ALL.
The study found that children who are genetically predisposed to producing high amounts of lymphocytes have a 20 percent or more increased risk of developing ALL. The study also shed light on the significance of the number of lymphocytes in proportion to other key blood cells.
“Ours was the first study to look for genetic variations associated with the ratio of lymphocytes to certain other blood cells – the ratio of lymphocytes to monocytes, the ratio of lymphocytes to neutrophils and the ratio of lymphocytes to platelets,” said de Smith. “It seems that it’s not just the genetic propensity to produce large numbers of lymphocytes, but it’s how those numbers relate to other blood cell types as well.”
Drawing from UK Biobank data from over 400,000 individuals, the researchers conducted a two-stage genome wide association study (GWAS) of blood cell traits, followed by analysis in 2,666 cases of ALL and more than 60,000 controls.
Data from the UK Biobank is from adults of European ancestry, but in the US, Latino children in particular are at higher risk of developing ALL than non-Latino children. In the future, de Smith hopes to focus blood cell trait research specifically on pediatric as well as Latino populations.
Primary and secondary DNA mutations leading to leukemia
ALL occurs when the DNA in bone marrow cell mutates. Normally cells grow and die at a set rate but with ALL, genetic mutations instruct bone marrow cells to continue growing and dividing. Blood cell production becomes out of control, and the bone marrow produces immature cells which develop into leukemic white blood cells called lymphoblasts. These abnormal cells are unable to fight infection and crowd out healthy white blood cells, red blood cells and platelets.
The disease is believed to be the result of two events. Up to one in twenty children are born with an initial genetic mutation known as a pre-leukemic clone. In most cases, these pre-leukemic cells never develop into leukemia. But, for children who develop ALL, a second mutation is triggered by biological events. A prevailing theory is that if a child’s immune system fails to develop properly, these secondary event mutations can occur, leading to leukemia.
The USC study outlines two hypotheses of how overproduction of lymphocytes could play a role in the events leading to leukemia. Children who are genetically predisposed to lymphocyte overproduction have an increased pool of pre-leukemic cells, and, subsequently, elevated chances of a secondary mutation occurring. A separate, but not mutually exclusive, hypothesis is that the overproduction of lymphocytes could factor into why the immune system fails to respond normally to infection in early life.
Risk scores for leukemia could lead to early prevention
The researchers’ theories correspond with the prevailing “delayed infection” theory of childhood leukemia and current research in preventing the onset of the disease. If children are not exposed enough to infections and microbes as infants, their immune systems may not be primed properly. To that end, researchers are developing probiotics as well as other potential interventions to prevent the secondary mutations leading to ALL.
In the future, de Smith envisions that a risk score may be assigned to newborns based on genetic risk factors including lymphocyte overproduction as well as non-genetic risks such as being born with a high birth weight or through a planned caesarean section. Children with high risk scores for ALL could receive early intervention therapies.
In keeping with this line of inquiry, de Smith will be involved in leading the largest study to date using new-born cord blood cells to investigate pre-leukemic clones in utero. Detecting the presence of these cells could also eventually be part of routine newborn screening for ALL risk and, ultimately, preventative measures.
About this study
Additional authors include first author Linda Kachuri and John S. Witte, University of California, San Francisco; Soyoung Jeon, Charleston W.K. Chiang and Joseph L. Wiemels, all of the Keck School; Andrew T. DeWan and Xiaomei Ma of Yale School of Public Health; and Catherine Metayer of University of California, Berkeley.
This study was supported by research grants from the National Institutes of Health (NIH) National Cancer Institute (NIC): R03CA245998 (AJD and LK), K99CA246076 (LK), R01CA155461 (JLW, XM) and R01CA175737 (JLK, XM).