Some people are better than others at recovering from a wounded heart, according to a new USC Stem Cell study published in Nature Genetics.
In the study, first author Michaela Patterson, a postdoctoral fellow in the laboratory of Henry Sucov, and her colleagues focused on a regenerative type of heart muscle cell called a mononuclear diploid cardiomyocyte (MNDCM). Zebrafish and newborn mammals, including mice and humans, have large numbers of MNDCMs and a relatively robust ability to regenerate heart muscle. However, adult mammals have few MNDCMs and a correspondingly limited capacity for regeneration after an injury such as a heart attack.
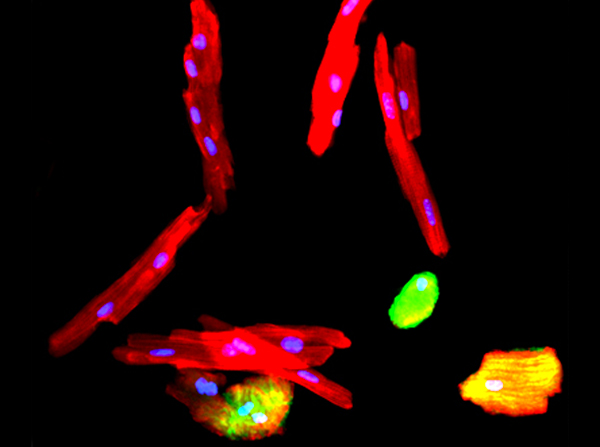
Heart muscle cells (red) with nuclei (blue). On the far right is a regenerative cell, which only has one nucleus, called a mononuclear diploid cardiomyocyte. (Image by Michaela Patterson)
Even so, the situation for adult mammals is not uniformly dire: Patterson and her co-authors observed a surprising amount variation in the number of MNDCMs among different strains of adult mice. In some strains, MNDCMs accounted for only 1.9 percent of heart muscle cells. In others, a full 10 percent were MNDCMs. As expected, the higher the percentage of MNDCMs, the better the mice fared in regenerating their heart muscle after injury.
“This was an exciting finding,” said Patterson. “It suggests that not all individuals are destined to permanent heart muscle loss after a heart attack, but rather some can naturally recover both heart muscle mass and function. If we can identify the genes that make some individuals better at it than others, then perhaps we can stimulate regeneration across the board.”
Using an approach called a genome-wide association study, the researchers indeed identified one of the key genes underlying this variation: Tnni3k. By blocking this gene in mice, the researchers produced higher percentages of MNDCMs and enhanced heart regeneration. In contrast, activating this gene in zebrafish decreased MNDCMs and impaired heart regeneration.
Sucov—senior author and professor of stem cell biology and regenerative medicine, integrative anatomical sciences, and biochemistry and molecular biology—described how this early discovery could be a first step towards a preventive strategy to mitigate heart disease, the leading cause of death in the Western world.
“The activity of this gene, Tnni3k, can be modulated by small molecules, which could be developed into prescription drugs in the future,” he said. “These small molecules could change the composition of the heart over time to contain more of these regenerative cells. This could improve the potential for regeneration in adult hearts, as a preventative strategy for those who may be at risk for heart failure.”
Additional co-authors include Lindsey Barske, Ben Van Handel, Peiheng Gan, Avneesh Sharma, Yukiko Yamaguchi, Hua Shen, Gage Crump, Hooman Allayee and S. Ram Kumar from USC; Ying Huang, Ching-Ling (Ellen) Lien and Takako Makita from Children’s Hospital Los Angeles; Christoph D. Rau, Aldons J. Lusis and Matt Denholtz from UCLA; and Shan Parikh and Thomas I. Force from Vanderbilt University.
Ninety percent of this work was supported by $1.08 million of private and non-federal funding from three sources: a Doerr Stem Cell Challenge Grant; an award from USC’s Provost Office; and a California Institute for Regenerative Medicine Training Grant (TG2-01161). Ten percent of the project was funded by $120,000 from National Institutes of Health grants (NHLBI NRSA 1F32HL124932, K08HL121191, HL123295, HL114137, and NS083265).