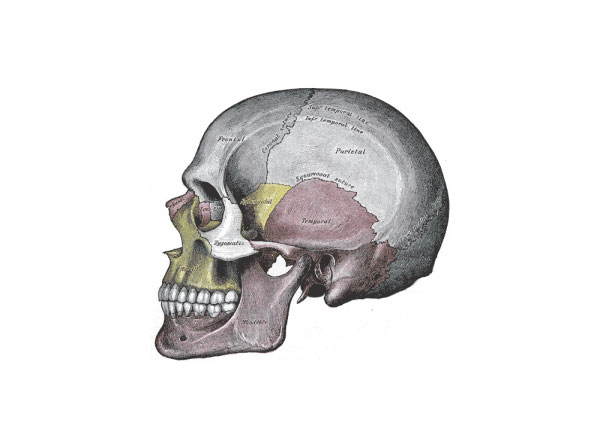
Human skull with sutures (Public domain image courtesy of Gray’s Anatomy)
It might surprise you to learn that your cranium is not one continuous smooth bone encasing your brain.
It’s actually comprised of eight bones, separated by fibrous joints, to give your skull flexibility. That’s the reason babies have “soft spots” and your brain was able to continue growing unabated throughout childhood.
With craniosynostosis—a birth defect estimated to occur in roughly one out of every 2,500 live births—the fibrous joints (or sutures) fuse together prematurely, leaving the cranium little room to expand to accommodate the growing brain. In a mild case, this may lead to a misshapen skull. In more severe cases, it can cause developmental delays, hearing loss, blindness and even death.
But maybe not for long, thanks to a $3.3 million grant from the National Institute of Dental and Craniofacial Research (NIDCR), which could eventually lead to more effective treatments.
“This is not just awesome funding,” said Yang Chai, associate dean of Research at the Herman Ostrow School of Dentistry of USC and one of three principal investigators on the study. “It also showcases what great collaborations can do, bringing three principal investigators together at this university so we can work on a complex problem like craniosynostosis.”
Joining Chai are Rob Maxson, professor of biochemistry and molecular biology, and Gage Crump, associate professor of stem cell biology and regenerative medicine, both from the Keck School of Medicine of USC.
With the five-year project, titled “Molecular and Cellular Basis of Craniosynostosis,” the three researchers will leverage their complementary expertise in craniosynostosis, stem cells, genetics and craniofacial bone development to better understand the genetic and molecular mechanisms behind suture development.
Stem Cells, Not Scalpels
At the center of the study are two genes called TWIST1 and TCF12, mutations of which have been discovered to contribute to craniosynostosis.
“Those genes really give us an entrée into the molecular and developmental processes that are going awry in craniosynostosis,” said Maxson, who helped to identify TWIST1 and TCF12’s role in suture development.
Not only will the scientists delete the two implicated genes during various stages of development using a mouse model, they will also observe the cranial suture fusion in zebrafish. Both animals develop craniosynostosis just like humans.
“The great thing about zebrafish is that they’re laid as one-cell embryos, they develop completely outside the mother, and they’re largely transparent,” said Crump, a zebrafish geneticist. “We can do live imaging on the fish to look at the bones as they’re developing and see what’s going wrong when the sutures fuse.”
By better understanding the genetic and molecular processes underpinning craniosynostosis, the researchers hope to one day develop biological interventions to treat craniosynostosis, rather than traditional surgical treatments, which often have to be done multiple times and have a high morbidity rate.
“It’s a very traumatic surgery,” Crump explained. “They take the whole skull cap off the child, fragment the bones and transplant the bones back into the skull.”
Crump said their research could eventually lead to a pharmacological intervention that compensates for the loss of the TWIST1 and TCF12 genes, which would keep the sutures open for normal brain development and make numerous surgeries unnecessary.
Greater than the Sum of the Parts
Each of the researchers brings decades of expertise to the study.
Chai is widely recognized throughout the dental and craniofacial research community for his investigations of the molecular and cellular mechanisms of craniofacial development, including oral and facial birth defects such as cleft palate. He is the director of USC’s Center for Craniofacial Molecular Biology.
In a Nature Cell Biology article published last year, Chai identified a population of stem cells that are required for long-term suture patency and calvarial bone growth.
Crump has pioneered live imaging techniques in zebrafish to examine the cellular basis of craniofacial defects. He is the principal investigator of the Crump Lab, which researches how genes affect bone and cartilage development in zebrafish.
Maxson has long-standing expertise in mouse models of synostosis, having contributed to the identification of TWIST1 and TCF12 as the two most affected genes in Saethre-Chotzen syndrome, a rare congenital disorder characterized by craniosynostosis. His lab also described the first mutation in people, MSX2, that causes craniosynostosis, in the 1990s.
Maxson and Chai have been collaborating on research for more than 20 years and together recruited Crump to USC.
“This study involves faculty members from two different schools, but we have a long history of very productive collaboration and a mutual trust that makes this venture possible,” Chai said.
“I think each one of us individually could have done something that would’ve been useful and interesting, but I think when you put the three of us together, there really is a synergism,” Maxson said. “I think there’s a good chance that we’ll do what this grant is intended to do and that is to come up with something where the whole is greater than the sum of the parts.”
Research reported in this publication was supported by the National Institute of Dental and Craniofacial Research of the National Institutes of Health under Award Number R01DE026339.
By John Hobbs