Longer pulses of electrical current allow patients to see focused spots of light
Retinal implants that deliver longer pulses of electrical current may noticeably improve image sharpness for individuals who have lost their sight due to retinitis pigmentosa, according to a new study by researchers from the USC Eye Institute and USC Viterbi School of Engineering.
The research will be published in the peer-reviewed journal Science Translational Medicine online on December 16.
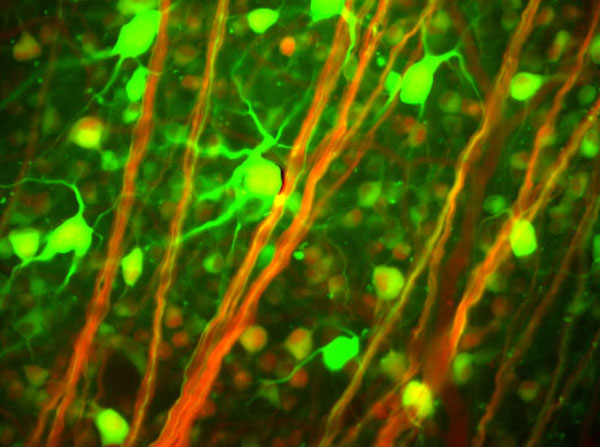
Retinitis pigmentosa (RP) is an inherited disease of the eye that causes blindness through gradual degeneration of photoreceptors, the light-sensing cells in the retina. The disease affects about one in 4,000 people. The Argus II retinal implant, also known as the ‘bionic eye’ was developed by a team of ophthalmologists and engineers at USC.
Retinal implants (artificial retinas) give people with RP the ability to perceive light, using a system that includes a video camera mounted on a pair of eyeglasses, a video processing unit that transforms images from the camera into wirelessly transmitted electronic signals, and an implanted array of electrodes to stimulate visual neurons.
Retinal implants have enabled blind individuals to detect motion and locate large objects. However, because the implants may unintentionally stimulate axons in the retina, patients sometimes see large oblong shapes of light that reduce the quality of their vision. In order for patients to see more clearly, the images created by the implant should be composed of focal spots of light.
Current implant technology stimulates the retina with brief pulses of electrical current roughly 0.5 millisecond (ms) in duration. The researchers found that increasing the duration of the stimulus pulses allows visualization of distinct focal spots of light.
“This is a huge step forward in helping restore sight for people with retinitis pigmentosa,” said Andrew Weitz, PhD, assistant professor of research ophthalmology. “Being able to create focused spots of light is important. Think of each light spot as a pixel in an image. By arranging many light spots into the shape of an object, we can generate sharp images of that object. For those of us who wear glasses, imagine the difference between trying to read a distant neon sign with and without your glasses on. For people with retinal implants, being able to see more clearly should have a big impact on their ability to recognize objects and navigate their environments. These improvements in vision can really boost a person’s sense of independence and confidence.”
The researchers tested various stimulus pulse durations in an animal model and validated their findings in a patient with an early version of the Argus retinal implant (Second Sight Medical Products, Inc.). The results indicated that longer pulse durations allowed the retina to be stimulated more precisely. In the animal model, all pulses 8 ms and shorter activated axons, obscuring the ability to generate a focal spot of light. Sixteen-millisecond pulses also stimulated axons but to a much lesser extent. Pulses 25 ms and longer produced no evidence of axonal stimulation, instead resulting in focal spots of light.
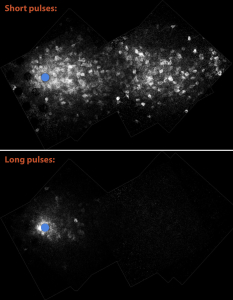
USC researchers found that longer pulse durations allowed the retina to be stimulated more precisely.
This research was conducted through a partnership between the USC Eye Institute and USC’s schools of medicine and engineering: the Viterbi School of Engineering Department of Biomedical Engineering and Ming Hsieh Department of Electrical Engineering; Keck School of Medicine’s Departments of Ophthalmology, and of Physiology and Biophysics; and device manufacturer Second Sight Medical Products Inc., in Sylmar, CA.
Researchers who contributed to the study include: Andrew C. Weitz (Department of Ophthalmology, Department of Biomedical Engineering); Devyani Nanduri (Department of Biomedical Engineering); Matthew R. Behrend (Ming Hsieh Department of Electrical Engineering); Alejandra Gonzalez-Calle (Department of Biomedical Engineering); Robert J. Greenberg (Second Sight Medical Products Inc.,); Mark S. Humayun (Department of Ophthalmology, Department of Biomedical Engineering); Robert H. Chow (Department of Physiology and Biophysics, Department of Biomedical Engineering); and James D. Weiland (Department of Ophthalmology, Department of Biomedical Engineering).
This research was funded in part by the National Science Foundation, National Institutes of Health (grants EY022931 and GM085791), Beckman Initiative for Macular Research, and Second Sight Medical Products Inc.
by Meg Aldrich