A study by the Keck School of Medicine of USC indicates that modulating the activity of a key immune receptor may prevent harmful hyper-inflammation in the immune system and may heal damage caused by osteoarthritis.
By Zara Abrams
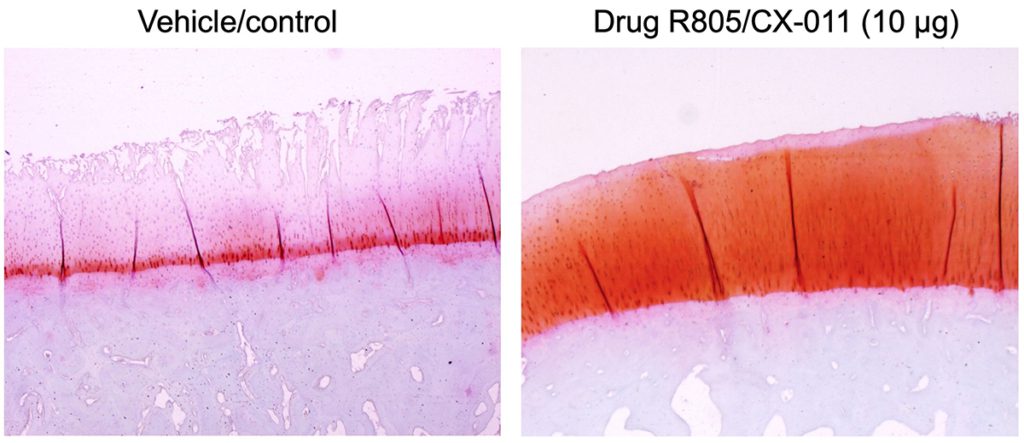
The image on the left shows damaged osteoarthritic cartilage without treatment in animal studies, and the image on the right shows regeneration of articular cartilage after knee injection of the new drug R805/CX-011. (Image: Evseenko Lab/USC Stem Cell)
A team of researchers at the Keck School of Medicine of USC have found a drug with the potential for curbing painful hyperinflammation from osteoarthritis, according to results of an animal study.
The findings, published March 22nd in Science Translational Medicine, indicate that a drug compound, R805/CX-011, may modulate an important cell receptor in the body’s immune system, GP130, that signals when antibodies should attack a virus or infection. The animal model studies showed that the drug compound can disrupt the receptor’s over-activation of inflammation, and still manage pain and stiffness.
“We saw a profound effect on joint pain, structure and function,” said Denis Evseenko, MD, PhD, a professor of orthopaedic surgery, stem cell research and regenerative medicine at the Keck School of Medicine.
The drug’s positive effects in mice and other animal models give researchers hope for its potential in upcoming trials with humans. This year, the team will launch a combined safety and preliminary efficacy clinical trial (Phases 1 and 2A) of R805/CX-011 for the treatment of osteoarthritis in patients in collaboration with the start-up Carthronix.
GP130: protector or mutineer?
GP130 in particular recruits white blood cells to launch the offensive against infection. However, it also summons the attackers in response to broken pieces of cartilage from our own joints — and to harmful effect. The consequence is hyper-inflammation in the joints — osteoarthritis — which causes debilitating chronic pain and stiffness for more than 32 million U.S. adults, according to the Centers for Disease Control and Prevention.
“In trying to fix the problem, the immune system causes even more damage,” said Evseenko. “But GP130 is a vital receptor. You cannot inhibit it, because it’s needed for healthy stem cells, as well as cardiovascular and immune function.”
Currently, there is no cure for osteoarthritis. Doctors may recommend physical therapy, exercise and weight loss to ease some symptoms, over-the-counter painkillers, or even joint replacement surgery.
Disrupting hyper-inflammation
The research by Evseenko and his colleagues suggests that blocking just one of GP130’s many signaling cascades, with either a drug or genetic modification, may prevent the hyper-inflammatory response that is the hallmark of osteoarthritis.
There also were signs in the animal models that the interventions could lead to tissue regeneration and healing, Evseenko said.
The researchers’ first step in the study was to show that they can halt the cellular processes behind the hyper-inflammation seen in osteoarthritis. To do this, the Genome Modification Facility at the Eli and Edythe Broad CIRM Center for Regenerative Medicine and Stem Cell Research at USC genetically modified a mouse, substituting one amino acid for another in a way that prevents a specific GP130 signaling cascade from being activated.
The mouse showed signs of resistance to arthritis. It also showed superior healing and regenerative capabilities compared to other mice. For example, instead of healing skin wounds with a scar, the mouse appeared to completely regenerate new skin, including hair follicles, glands and other skin substructures.
“No white blood cells rushed to the scene and no hyper-inflammation occurred,” Evseenko said.
Next, Evseenko collaborated with Mark Hurtig, a doctor of veterinary medicine, and his colleagues at the University of Guelph’s Ontario Veterinary College to test R805/CX-011 in small and large animal models of osteoarthritis.
The double-blind study mimicked a human clinical trial. The researchers tested the drug’s effects in three different doses, then compared those to a placebo control group.
In addition to the reduction in joint pain, and effect on structure and function, the results also showed a clear “dose-dependent effect” that is critical for drug efficacy, Evseenko said.
Next steps: Phases 1 and 2A Trials

Denis Evseenko, MD, PhD, and Jay Lieberman, MD, Keck School of Medicine of USC. (Photo: Sergio Bianco)
The new drug, an advanced version of a previously discovered compound RCGD423 that targets GP130, will be tested in an upcoming phase 1 and 2A clinical trial. Evseenko, Jay Lieberman, MD, chair and professor of orthopaedic surgery at the Keck School of Medicine and a co-author of the study, and the Carthronix team have received more than $5 million from the Department of Defense to fund the research, which will test R805/CX-011 knee injections in up to 70 patients.
Currently, many osteoarthritis patients receive only physical therapy and non-steroidal anti-inflammatory drugs to manage the condition. But those remedies often are not enough to restore function and eliminate the severe pain caused by osteophytes, tiny bone spikes that grow on chronically inflamed joints. An estimated 3% of osteoarthritis patients—around 1 million people in the U.S. alone—become addicted to opioids as a result.
Injections of R805/CX-011 may offer a less expensive, less invasive option that could be delivered several times a year in an outpatient clinic. It has the potential to delay or even reduce the need for joint replacement surgery, the only existing FDA-approved therapy for osteoarthritis.
The researchers also plan to explore the efficacy of R805/CX-011 for stimulating tissue regeneration in a broad range of other medical conditions, including pulmonary fibrosis and bone loss resulting from chronic obesity.
(Disclosure: Denis Evseenko and Ben Van Handel are co-founders and shareholders of Carthronix Inc.)
About this study
In addition to Evseenko, Hurtig and Lieberman, the study’s other authors are Ruzanna Shkhyan, Arijita Sarkar, Ben Van Handel, Jinxiu Li, Jesse York, Nicholas Banks, Robert Van der Horst, Nancy Q. Liu, Siyoung Lee, Jade Tassey and Thomas Lozito from the Departments of Orthopaedic Surgery and Stem Cell Biology and Regenerative Medicine, Keck School of Medicine of USC; Candace Flynn and Emma Lamoure from the Department of Clinical Studies, Ontario Veterinary College, University of Guelph; Paul Bajaj and Kanagasabai Vadivel from the Department of Orthopaedic Surgery, David Geffen School of Medicine, UCLA; and Hans I-Chen Harn from the Department of Pathology, Keck School of Medicine of USC and the International Research Center of Wound Repair and Regeneration, National Cheng Kung University, Taiwan.
This work was supported by the U.S. Department of Defense [W81XWH-13-1-0465]; the National Institutes of Health [R01AR071734, R01AG058624, U24DE026914, R01GM125322]; and China Medical University in Taiwan-University of Southern California research contract 005884. A donation from Carrol and R. Rex Parris also supported this line of research.