(Originally posted at USC Schaeffer.)
By Stephanie Hedt
One year into the pandemic, it is still unclear what the effects of the coronavirus and stay-at-home orders have been on healthcare utilization and patients seeking care unrelated to COVID-19 symptoms.
In a new study, researchers examine the impact of the first stay-at-home order in L.A. County on emergency department use at LAC+USC medical center- one of the busiest emergency departments in the country.
Published in the Western Journal of Emergency Medicine, the study found immediately after Los Angeles’ safer-at-home declaration, emergency department utilization dropped by 37% compared to the same 9 weeks in the prior two years. This drop was seen regardless of the severity of the diagnosis or demographics of the patient. Patients with higher needs and those that were older, male, black, uninsured, and publicly insured accounted for a disproportionate share of the remaining ED use.
“Whether or not patients were foregoing care and who these patients were is important to understand,” explained Sarah Axeen, a fellow at the USC Schaeffer Center and assistant research professor at the Keck School of Medicine of USC. “The media and colleagues gave anecdotal evidence at the start of COVID about significant drops in patients but we wanted to quantify what the magnitude actually was.”
Why it matters who stayed at home
COVID has impacted all aspects of our lives, including how we deliver healthcare. Understanding the impact of COVID-19 stay-at-home orders on the operations of a large, public emergency department is important given the potential health consequences for these patients who have delayed care and in planning for future pandemics.
“We learned that during the initial phase of the COVID pandemic in Los Angeles, people stopped coming to the emergency department,” said Schaeffer Center Clinical Fellow Michael Menchine. “While some of this reduction may have helped protect people from contracting COVID in the hospital setting, we certainly worry that vulnerable people with severe conditions are staying home and that this could lead to poor health outcomes.” Menchine is an Associate Professor of Clinical Emergency Medicine at the Keck School of Medicine of USC.
The researchers developed a dataset of weekly ED visits for the first 18 weeks of the year (January to early May) in 2018, 2019, and 2020. This four-and-a-half-month period includes the general peak and downturn of influenza seasons, as well as the initial outbreak and slowdown of COVID-19 in LA. County and the corresponding stay-at-home order.
Overall, the LAC+USC Medical Center ED had approximately 56,000 total patient encounters in the first 18 weeks each year during 2018 and 2019. In 2020, that total number reduced by almost 20% to 45,488. Nearly all the declines came in the second half of the observation period, tracking with the outbreak of COVID-19 and the safer-at-home directives. The ED visit reductions were geographically uniformly distributed across Los Angeles County.
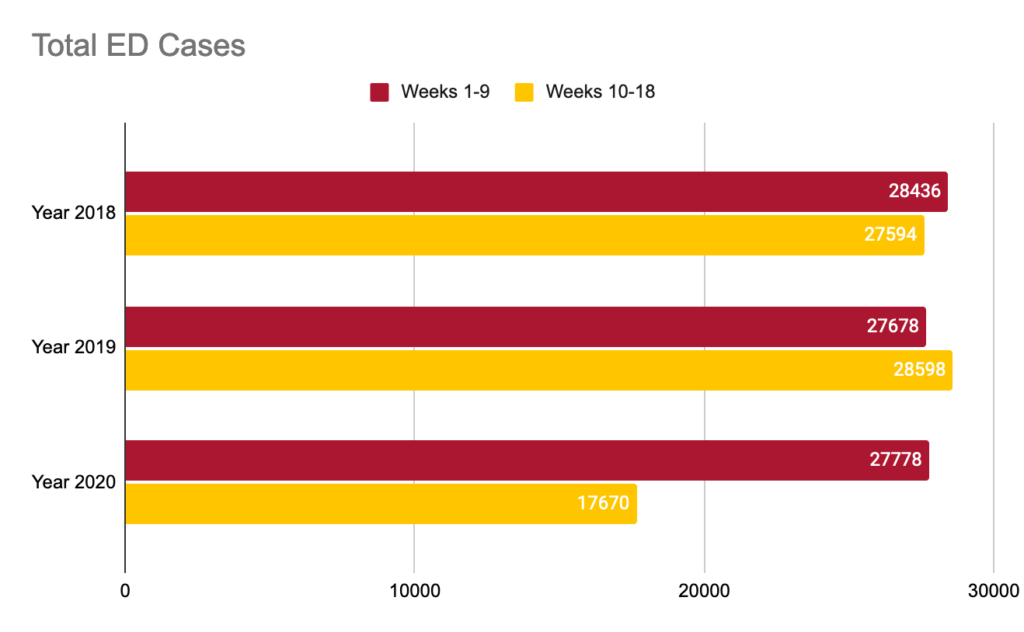
The only patient group who saw an increase in the number of ED encounters were patients diagnosed with a COVID-related disease of the respiratory system. In the first 9 weeks of 2020 there were more respiratory cases than average compared to the previous two years, showing a 20-34% increase depending on the year. After the safer-at-home orders, visits by even patients with respiratory illnesses decreased, though the decrease was concentrated in patients with relatively mild rather than severe respiratory diagnoses.
“We found that even in the final week of our observation window—nearly 10 weeks after the safer-at-home declaration—there were still 1,000 fewer visits to the ED compared to the same week in prior years,” explained Axeen. “As patients continue to forego care, perhaps due to a fear of COVID exposure or to a fear of violating safer-at-home orders, policymakers and practitioners need to find ways to proactively reach out to these patients to ensure that either through telehealth or non-acute health care settings they are able to obtain necessary care.”
The author’s findings point to an abrupt, discontinuous impact of COVID-19 on ED utilization. While the second stay-at-home order has had an undoubtedly different impact on ED capacity, these findings highlight an important trend that may have long-term impacts on patient outcomes and the health of the community.
In addition to Axeen and Menchine, study authors include Chun Nok Lam, Sophie Terp, Elizabeth Burner, Dan Dworkis, and Sanjay A.Arora.
