
Rosemary Navarro, 40, at her home in La Habra, Calif. Navarro looks through old childhood photographs to find a picture of her mother, Rosa Maria Navarro, who also had the familial Alzheimer’s. (Heidi de Marco/Kaiser Health News)
Rosemary Navarro was living in Mexico when her brother called from California. Something wasn’t right with their mom, then in her early 40s. She was having trouble paying bills and keeping jobs as a food preparer in convalescent homes.
Navarro, then 22, sold her furniture to pay for a trip back to the U.S. for herself and her two young children. Almost as soon as she arrived, she knew her mother wasn’t the same person. “She was there but sometimes she wasn’t there,” she said. “I thought, ‘Oh man this isn’t going to be good.’”
Before long, Navarro was feeding her mom, then changing her diapers. She put a special lock on the door to keep her from straying out. Unable to continue caring for her, Navarro eventually moved her to a nursing home, where she spent eight years.
Near the end, her mom, a quiet woman who had immigrated to the U.S. as a teenager and loved telenovelas, could communicate only by laughing or crying. Navarro was there when she took her last breath in 2009, at age 53. “What I went through with my mom I wouldn’t wish on anyone,” she said.
It has happened again and again in her family — relatives struck by the same terrible disease, most without any clue what it was. An aunt, an uncle, a cousin, a grandfather, a great grandfather. “Too many have died,” Navarro said. All in their early 50s.
Now the family knows the reason for their curse: It’s a rare type of early-onset Alzheimer’s disease, caused by what’s come to be known as the “Jalisco” genetic mutation. Doctors today can tell someone they have it but they can’t stop its destructive march.
For Navarro, watching her relatives succumb is like looking into a crystal ball, one she wants to hurl across the room.
She, too, has the mutation.
It’s getting harder to stifle her fear. In April, she turned 40 — the same age her mother was when she started wandering off and forgetting simple things.
“I don’t look forward to birthdays,” she said. “I didn’t want to celebrate 40, much less 41.”
Sparing The Next Generation
Navarro, who lives in La Habra, Calif., belongs to an exclusive but unenviable club whose members are genetically programmed for early memory loss and death.
Of the more than 5 million people across the U.S. who have Alzheimer’s, 5 percent are believed to have the early-onset form, striking people under the age of 65. Fewer still — about 1 percent — have genetic mutations that are known to cause the disease.
Navarro’s gene is known as the Jalisco mutation because it is believed to have surfaced first in that Mexican state. Passed from parent to child over generations, it likely was carried by immigrants across the Mexican border into California and other states. In Mexico and the U.S., roughly 50 families are known to have the mutation.
Cases like Navarro’s are of great interest to Alzheimer’s researchers. Studying this unique population with genetic mutations, they say, could help unlock some of the biggest mysteries of the more common form of the disease: How does it develop? How can it be diagnosed earlier? What can be done to stop it?

A photograph of Rosemary Navarro’s mother, Rosa Maria Navarro, sits on her dining room table. Navarro’s mother died in 2009 from Alzheimer’s disease. “What I went through with my mom I wouldn’t wish on anyone,” Navarro said. (Heidi de Marco/KHN)
Ordinarily, it’s difficult — if not impossible — to predict Alzheimer’s. But with these families, researchers know the mutation carriers will get the disease. They also know approximately when symptoms will appear. So they can get a real-time look at how the disease develops — and can measure when the brain starts changing relative to expected onset. Perhaps most important, they can design drugs to target the disease before patients lose their memory.
“If you know from age 18 or even from birth whether someone is going to develop the disease or not, you have got a big window to intervene,” Navarro’s doctor, John Ringman, a neurology professor at the Keck School of Medicine of the University of Southern California. “We don’t have a way to repair or bring back lost brain cells.”
Already, researchers of inherited Alzheimer’s have discovered clues that could lead to potential treatment for all patients with the disease. They have determined, for example, that the formation of amyloid plaques characteristic of Alzheimer’s appear decades before the first noticeable signs of memory loss, and they recently began testing whether medications can block those plaques from forming in the brain.
Patients with a familial Alzheimer’s mutation “are sort of a model for how the disease progresses, because they are easier to recognize and easier to study,” said Bruce Miller, a longtime Alzheimer’s researcher who directs the memory and aging center at the University of California, San Francisco.
Around the world, hundreds of people whose families are afflicted with a variety of early-onset mutations are subjecting themselves to medical tests — spinal taps, memory quizzes, MRIs and other brain imaging, hoping scientists can develop therapies to prevent and treat Alzheimer’s.
But their participation often comes with the sad realization that resulting treatments may come too late for them. Ringman is studying about 100 patients at USC. Navarro is among about 30 with the Jalisco mutation.
More than 450 people are part of an international network of research being led by Washington University School of Medicine in St. Louis. Each has a parent with an early-onset gene mutation. If the research doesn’t help them, they tell researchers, maybe it will help the next generation.
“They are all desperately fearful that they themselves have inherited a mutation,” said John C. Morris, director of the school’s Alzheimer’s Disease Research Center. “But what they are really fearful about is that if they did, that they will pass it along to their children.”
Children have a 50 percent chance of inheriting the mutation from a parent who carries it.
Navarro is well aware of the statistics. She has joined the network’s research effort, of which Ringman is a part. She did it not just for herself but for her family — including her two children, now young adults.
Last year, she went for a brain scan. She had no overt symptoms, but the results told a different story. Her brain had already started to shrink — a sign that the disease was taking hold.
‘At Least We Know Now’
In November 2015, Dr. Ringman drove to Colton, Calif. — 60 miles east of Los Angeles — to meet with the large and close-knit Kitchen family. Jay Kitchen and his younger brother John had been referred to him after each suffered a series of baffling symptoms.
It had started about four years earlier. Jay, then a 44-year-old sports writer, began having difficulty speaking. He felt off balance, was forgetting things and having difficulty paying bills.
Soon afterward, his younger brother, John, a high school history teacher, started becoming easily confused. He would forget what day it was and how to get to the market.
“It struck me as really odd,” said John’s wife, Michelle Lopez. “Nobody could forget the store that was around the corner from the house you lived in for 12 years.”

John and Jay Kitchen with their father in Colton, California, on December 10, 2015. (Heidi de Marco/KHN)
Lopez said John started taking illegal drugs. At one point, while they were separated, he was arrested for stalking her. His bizarre behavior, completely uncharacteristic of him, nearly broke up their marriage, she said.
Jay Kitchen was the first to seek help. He went to an emergency room, then several specialists. One suspected a stroke. Another suggested mental illness. Test after test came back negative or inconclusive.
“It has been a long haul trying to get a diagnosis,” said the brothers’ aunt, Linda Ramos, who took Jay Kitchen to most of the appointments. Doctors constantly were “scratching their heads trying to figure out what was wrong.”
Late in 2015, a neurologist referred the brothers to Ringman, who ordered a blood test.
On the November morning in Colton, Ringman arrived at Ramos’ home, where the extended family was gathered. He pulled the brothers and a few others aside to deliver his grim news: Both men had the Jalisco mutation. Ramos said the brothers sat in near silence. She doesn’t think Jay understood, and John, already a quiet man, just seemed scared.
Later that morning, a larger group of family members met with Ringman around a long dining room table: the Kitchens’ father, aunts and uncles; Lopez and Jay Kitchen’s ex-wife. Jay Kitchen’s son came with his newborn, who fussed in a stroller.
Projecting pictures and diagrams on the wall, the doctor explained, in his matter-of-fact way, the history and science behind early-onset Alzheimer’s disease and the different types of mutations that can cause it.

John Ringman, a neurologist at the University of Southern California, gives a presentation on the alzheimer mutation for John and Jay Kitchen’s family in Riverside, California, on Sunday, November 22, 2015. Ringman has devoted much of his career studying families with the mutation. (Heidi de Marco/KHN)
Medications available today only address the symptoms, not the disease itself, Ringman said. Drugs may improve people’s thinking but don’t stop the progression.
“This is something we are going to crack eventually,” he said.
Like many families Ringman encounters, the relatives in the dining room absorbed the news with little emotion or surprise — as though the doctor were confirming nameless fears.
Ramos had watched the Kitchens’ mother, Olivia, lose the ability to walk and speak and eventually die in 2002. At the time, they were told she had multiple sclerosis. Now she was not so sure.
John Kitchen asked if there was any connection to Huntington’s disease, which the family had been told his grandfather had.
“Probably he didn’t have Huntington’s,” Ringman responded, adding that people are sometimes misdiagnosed.
Ramos recalls feeling somewhat relieved that day.
“My thought was, ‘At least we know now. Finally, we know. Thank God we have a name
One Family Leads To Another
In John Ringman’s office at the University of Southern California in Los Angeles, the shelves are filled with volumes on neurology and memory, accompanied by a model of the brain and a Sigmund Freud doll.
Ringman, though sometimes gruff, betrays a wry humor and a deep passion for science. He easily recalls patients’ stories over the years.
For the 51-year-old neurologist, who has two young children, working with families predestined to forget their own stories and die young can be “very depressing.” “It doesn’t get easier to be delivering the bad news,” he said.
At the same time, he likes getting to know his patients and watching their children grow up.
He became interested in neuroscience while in college at the University of California, Berkeley. But he knew lab work wasn’t for him. “I realized all these Ph.D.s study one molecule their entire lives and sit in a laboratory,” he said. “I didn’t want that.”
In the late 1990s, after completing medical school and specialty training, he joined the medical staff at the University of California, Irvine, where he saw patients with dementia and Huntington’s disease. He liked the personal interaction, combined with the scientific challenge.
In 1999, a 42-year-old woman came to see him, brought in by her young adult daughter. Rosa Maria Navarro had signs of early Alzheimer’s disease. Her daughter Rosemary was distraught, reporting that something similar had afflicted many other relatives.
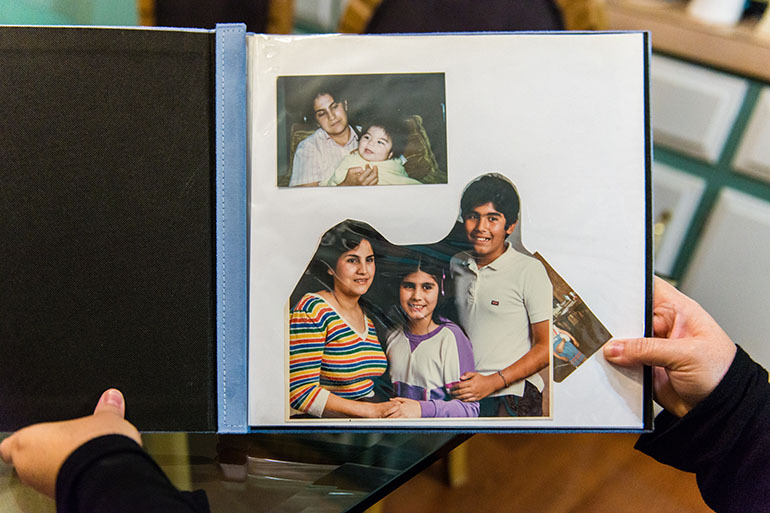
Rosemary Navarro, 40, at her home in La Habra, California, on Monday, December 22, 2016. Navarro looks through old childhood photographs to find a picture of her mother, Rosa Maria Navarro, who also had the familial Alzheimer’s. (Heidi de Marco/KHN)
It was the beginning of a long relationship, and a new line of scientific inquiry for Ringman.
The young neurologist was aware of recently identified familial Alzheimer’s mutations, and he immediately suspected Rosa Maria had one. He sent her blood sample to get the genetic test, and it came back positive for the A431E mutation of a gene known as presenilin 1.
Rosemary Navarro suspects her mother sensed even before then what was wrong, having seen her own father lose his memory and die young. “But she was quiet,” Navarro said. “She never said, ‘I might have this.’”
Soon afterward, another patient came into Ringman’s office with similar symptoms. That patient tested positive for the same mutation. Both had families originating from Jalisco, Mexico. “I was already getting suspicious,” he said.
Familial Alzheimer’s intrigued Ringman. It was a relatively new field. Families with the disease had been known to exist since Alzheimer’s first described the disease in 1906, but the genes weren’t identified until about 90 years later. The research touched on so many parts of science — neurology, biology and psychology.
Later, Ringman came across an article co-authored by a Mexican neuropsychologist he had worked with before, Yaneth Rodriguez. It was about four families in Mexico that had early Alzheimer’s disease, and they had symptoms similar to his two patients.
In 2000, Ringman traveled to Mexico and met with both Rodriguez and a geneticist, Maria Elisa Alonso. Alonso told him that another family there had tested positive for the A431E mutation. Now, there were three, all of Mexican heritage.
Ringman collected DNA samples of members of seven more families who were being treated in Mexico. Test results not only confirmed members of each family had A431E, they indicated the patients all shared the same chunk of DNA. That’s when he knew. They were all related, distant cousins who had never met.
Over the next few years, Ringman saw more and more patients with relatives from Jalisco and symptoms of memory loss at about age 40. In addition to their cognitive problems, they sometimes suffered from leg stiffness and fleeting seizures.
In 2006, the Mexican geneticist, Alonso, published a report in Neurogenetics, describing nine families who didn’t know they were related but all shared the A431E mutation. She concluded that the disease likely started with one ancestor in Jalisco. Ringman published a response describing 15 additional families with the same mutation.
The findings meant that Ringman’s patients owed their suffering to an unidentified individual who likely lived in Jalisco perhaps hundreds of years ago. Somehow, as his or her DNA copied itself during cell division, a fatal mistake occurred. And now, in places like La Habra and Colton, Calif., whole families were coping with the awful results.

Relatives gathered around a dining room table as neurologist John Ringman gave a presentation about Alzheimer’s disease and current research in Riverside, California, on Sunday, November 22, 2015. (Heidi de Marco/KHN)
Meanwhile, other scientists around the world had found families with different early-onset mutations in one of three identified genes, including a group in Puerto Rico and one in Colombia. Each group was believed to share a common ancestor.
Ringman saw the tragedy but also the scientific opportunity in these discoveries.
He worked on his Spanish and delved deeper into the cases on both sides of the border. He published reports on specific characteristics of Jalisco mutation carriers, such as the leg stiffness and weakness called spastic paraparesis. He described biochemical changes at the very early stages of the disease, such as changes in beta amyloid and tau, protein associated with Alzheimer’s, in the cerebral spinal fluid. And he reported how cognitive decline among carriers was similar to those with late-onset Alzheimer’s.
Ringman is continuing to identify new patients with familial Alzheimer’s. Some are referred by doctors in the U.S. and some by doctors in Mexico. He helps people get tested for free when they suspect the Jalisco mutation.
“Some people have no idea that there is a genetic test for this,” he said.
In homes across Jalisco, he and Rodriguez’s team are educating families about the disease — so that they will be informed enough to participate in future clinical drug trials. Some take comfort from helping with the research. Some have decided not to have children.
Ultimately, Ringman joined the Washington University School of Medicine network in its international quest for knowledge and treatment options for familial Alzheimer’s disease. The research now includes different sites in Europe, Asia and Australia.
The formal name is the Dominantly Inherited Alzheimer’s Network, because the gene is passed down from one parent. USC is one of the research sites.
The network’s investigators — who all use the same standardized measures — are monitoring biological changes among carriers and non-carriers and are testing medications.
In addition to finding the early emergence of amyloid plaques, researchers have discovered decreased beta-amyloid peptides and increased tau proteins in spinal fluid 15 years before symptoms appear. Measurable shrinkage in some parts of the brain also occurs five years before symptoms.
The research essentially has presented a timeline of brain changes leading up to memory loss and cognitive decline and has helped lead scientists to decide when and where to aim drugs.
A promising target is beta amyloid. Many researchers believe that flaws in how the sticky substance is accumulated and disposed of in the brain can lead to the disease.
Scientists are studying two drugs aimed at attacking beta amyloid, with the equally unpronounceable names of Gantenerumab and Solanezumab. Both are antibodies that bind to the beta amyloid and help remove it from the brain.
Another encouraging finding, the researchers say, is that early-onset and late-onset Alzheimer’s seem to share many characteristics, and findings that help with one disease are likely to help with the other.
‘Praying For A Miracle’
Neither of the Kitchen brothers is participating in the research. Both are in precipitous decline.
As John’s symptom’s worsened, Michelle Lopez invited him to move back in with her and their son, Reese, who is 14.
John, now 43, can still hold a conversation, but he struggles to find the right words. He gets frustrated at his inability to do simple tasks, like write his own name. He feels he is losing control of his life and worries about his family. “I want to be around for my son,” he said.
Lopez said she’s happy to have him back home. She is still “praying for a miracle.”
The changes have been hard to watch — and not just for her. Within a week after John moved back into the house, Reese asked his mom, “Is that going to happen to me?”
“That was the worst day of my life,” Lopez said.

Michelle Lopez, John Kitchen’s wife, tears up after the Alzheimer’s presentation in Colton, California, on Sunday, November 22, 2015. Lopez says she is relieved to finally have a diagnosis for the disease that is destroying her family. (Heidi de Marco/KHN)
Reese said his dad forgets things easily. “It’s like very slowly he is fading away.”
Reese tries not to think too much about his dad’s disease or what the mutation could mean for his own life. Lopez said Reese will wait until he becomes an adult to decide whether or not to get tested. Right now, he just focuses on school and helping his mom and dad.
John takes one medication, donepezil, used in many later onset Alzheimer’s patients to improve cognition and behavior. The neurologist recently told them it may only prolong cognitive abilities a month longer. “That was disheartening to hear,” Lopez said.
In December 2015, relatives realized Jay Kitchen could no longer live on his own. They arranged for him to rent a room from a friend. But soon after, he couldn’t figure out how to open a door and climbed, barefoot, out of the window.
He told relatives people were trying to kill him. Alarmed by the paranoia, the family took him to the emergency room. The family decided to place him in a nursing home but he scaled a fence and left without telling anyone.
“We were flabbergasted,” said his aunt, Linda Ramos. “We don’t know what to anticipate — is it all downhill from here? It all seems incredibly quick.”
Now, Jay Kitchen is in a locked facility. He recognizes family only occasionally and regularly misplaces his belongings. He can no longer speak in complete sentences and has trouble getting dressed.
“We get a glimmer of hope, but then we think we are foolish for even hoping,” Ramos said. “This is just devastating. It’s a horrible disease.”
Fear And Faith
Navarro’s 19-year-old daughter, Lizeth, and her 22-year-old son, Ricardo, live with her in a three-bedroom trailer in La Habra. They depend heavily on her, emotionally and financially.
Both say their mom has started forgetting little things — the movie they saw last week or what they need from the grocery store. “I usually have to say things more than once,” said Lizeth Navarro.

Rosemary Navarro’s 22-year-old son, Ricardo, and her 19-year-old daughter, Lizeth, live with her in a three-bedroom trailer in La Habra, California. They depend heavily on her, both emotionally and financially. (Heidi de Marco/KHN)
Lizeth, a chemical engineering major, decided to attend college nearby partly just to keep an eye on her mother. She hasn’t decided whether to get tested for the mutation herself. But her brother said he won’t.
“I would rather live my life not knowing,” said Ricardo Navarro, who is studying broadcast journalism at the California State University, Fullerton. “What is the point of living my life if I know I am going to die in my 40s or 50s?”
Their mother, meanwhile, works in customer service. She doesn’t make a point of telling employers about her condition. At a recent temp job, she had trouble focusing and remembering some of the things her trainers taught her. She didn’t get hired on permanently.
Navarro tries to focus on her family rather than the disease. “I can’t let it overcome me,” she said.
She puts a lot of hope in a drug trial out of Washington University. Each month, a nurse visits her in La Habra and injects a medication, which she’s pretty sure is not a placebo.
“I have to have faith in the drug,” she said. “That’s my only solution for now.”
“Otherwise …”
She didn’t finish her thought.
By Anna Gorman, Kaiser Health News
Photos by Heidi de Marco
Kaiser Health News is an editorially independent program of the Henry J. Kaiser Family Foundation, a nonprofit, nonpartisan health policy research and communication organization not affiliated with Kaiser Permanente. KHN’s coverage in California is funded in part by Blue Shield of California Foundation. This story was also shared by NPR.